Self Empowerment Resources
RACE Line Request
If you are admitted to a hospital or involved in outpatient care with non-ED specialized clinicians, request that the provincial RACE line services be contacted to advise care decisions. Make sure to request that if the RACE line is not contacted, this is charted in your medical records.
RACE Line Information
Clinicians can contact RACE support lines for St. Paul’s Eating Disorder Program for internal medicine, psychiatric, nursing, and dietetic advice (there are multiple provincial protocols on various ED related treatment concerns.)
RACE Phone Line
Monday to Friday 0800-1700
Local Calls: 604-696-2131
Toll Free: 1-877-696-2131
RACE website - http://www.raceconnect.ca/contact-us/
Fillable Templates
The following templates are downloadable so that you can individualize them for your own care needs. These documents are designed for inpatient settings (e.g. going into treatment or when in hospital, but can be adapted to outpatient settings as well.)
Care Planning Template
This template is specifically designed to support trauma-informed approaches to care as identified by an individual and based on their unique needs. It looks at a person’s identified need or a challenging situation, environmental stressors or triggering factors, what the goal would be in a situation the person becomes escalated, and the interventions that they typically find supportive.
For example:
Identified Need/Challenging Situation - Overstimulation triggering a state of hyper-arousal (fight, flight)
Environmental Stressors/Triggering Factors - Limited personal space, people trying to have a conversation when the individual is hyper-aroused, noise, lack of quiet spaces and privacy, a locked ward with nowhere to go, certain noises/sounds, shared rooms
Goal - individual is able to ground themselves and utilize coping skills
Supportive Interventions - earplugs, music, individual is able to leave the space and go somewhere quiet, grounding objects, individual is able to go outside briefly, staff check in every so often to ensure safety, but wait for the person to come to them when ready, the focus of care shifts from “this needs to be done” to “this person needs space to ground before we can re-approach this conversation or aspect of care.”
The template can be found here.
Goals Template
This template outlines basic overall goals (again it’s designed more for an admission to a treatment facility or during an inpatient stay, but can easily be adapted to outpatient work or everyday life). The categories of goals provided include: nutritional, self-care/leisure, interpersonal, and psychological (however these can be changed as needed).
The template can be found here.
Safety Plan Template
For those who have had many a safety plan thrown their way, these documents can feel useless. This best safety plan is one that is useful to you (if it is useful to you) and as such, we highly recommend individualizing this document and sharing it with your loved ones, support network, and any professionals you are working with. The last row looks at “ways to be supportive as a loved one or healthcare professional.” In this space it can be helpful to outline exactly what your preferences similar to an advanced care planning type of document. If you are in crisis, what are the most supportive things to do in a step-wise fashion?
For example, if you have negative experiences with being detained by police you could outline avoiding police and utilizing a local PACT (peer assisted crisis team) number instead if there is one available in your community (see CMHA BC for details on local PACTs). If you have a safe support network that can do something akin to “pod mapping,” can those persons be utilized. If you do have to brought to a psychiatric emergency service, what are the key things you would want a care provider or loved one to communicate about your care needs to that healthcare facility?
The template can be found here.
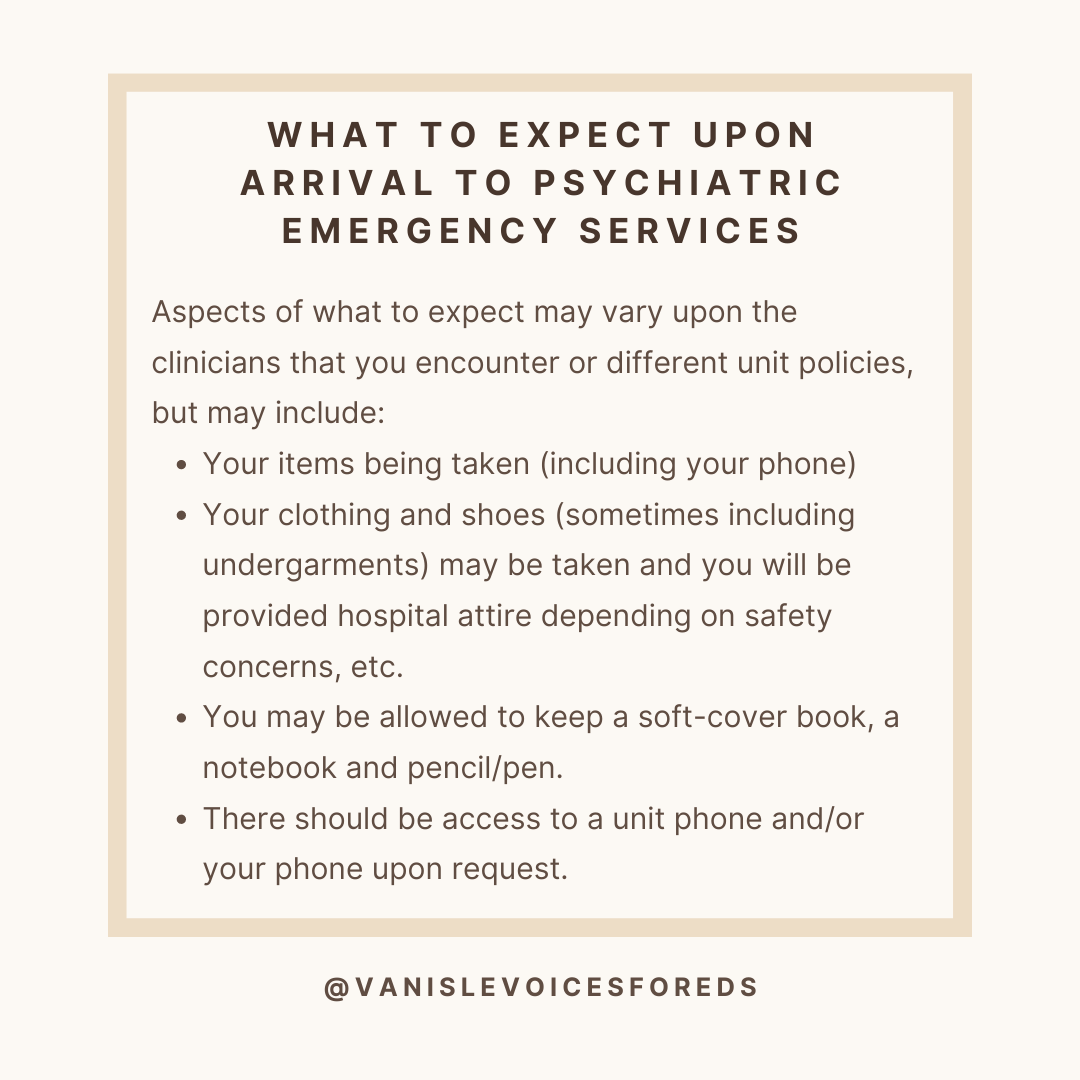
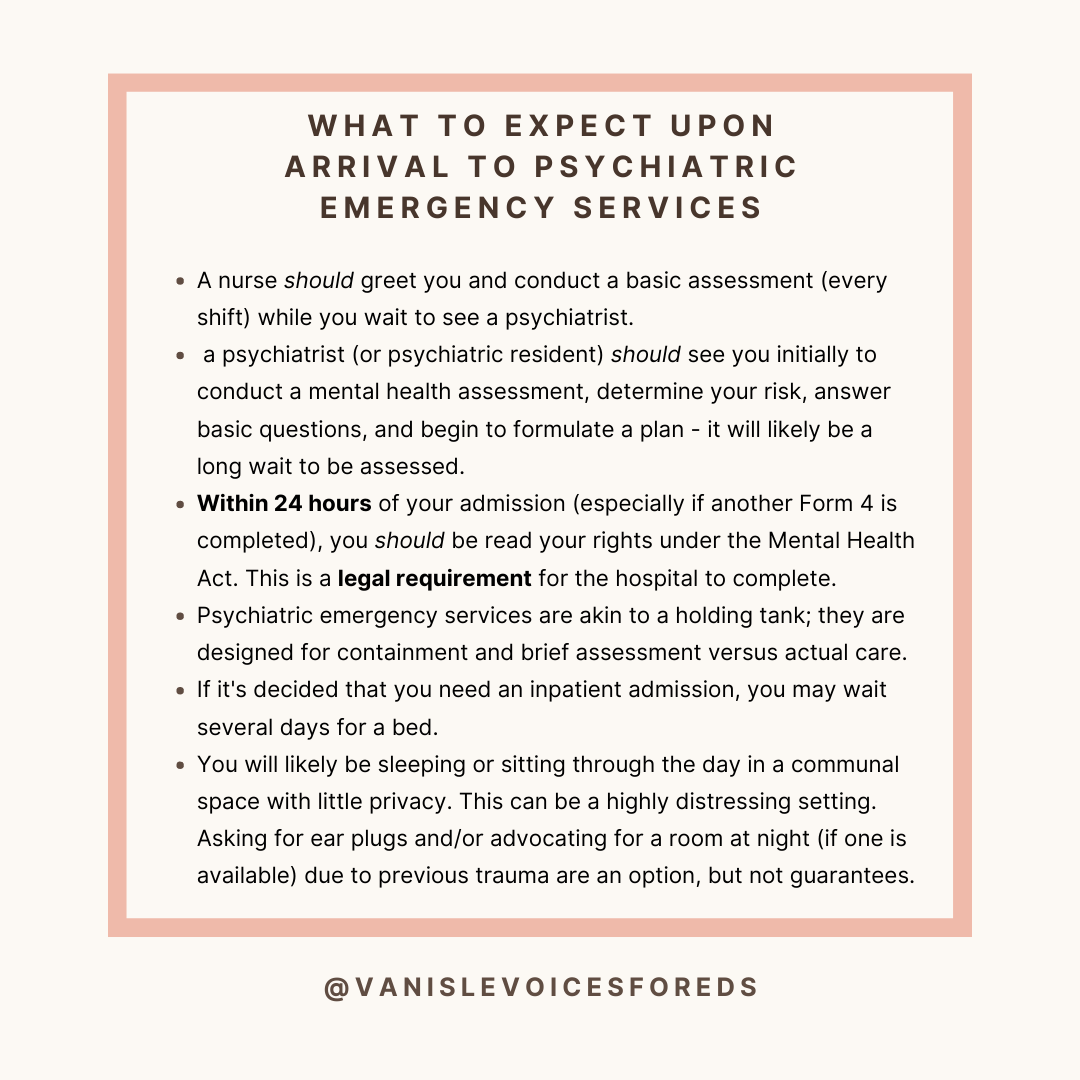
Basic Psychiatric Services Survival Guide
The Mental Health Act in British Columbia (B.C.) was passed in 1964. Important sections of this Act to note include the following:
Section 28 (1) - A police officer or constable may apprehend and immediately take a person to a physician or nurse practitioner for examination if satisfied from personal observations, or information received, that the person (a) is acting in a manner likely to endanger that person's own safety or the safety of others, and (b) is apparently a person with a mental disorder.
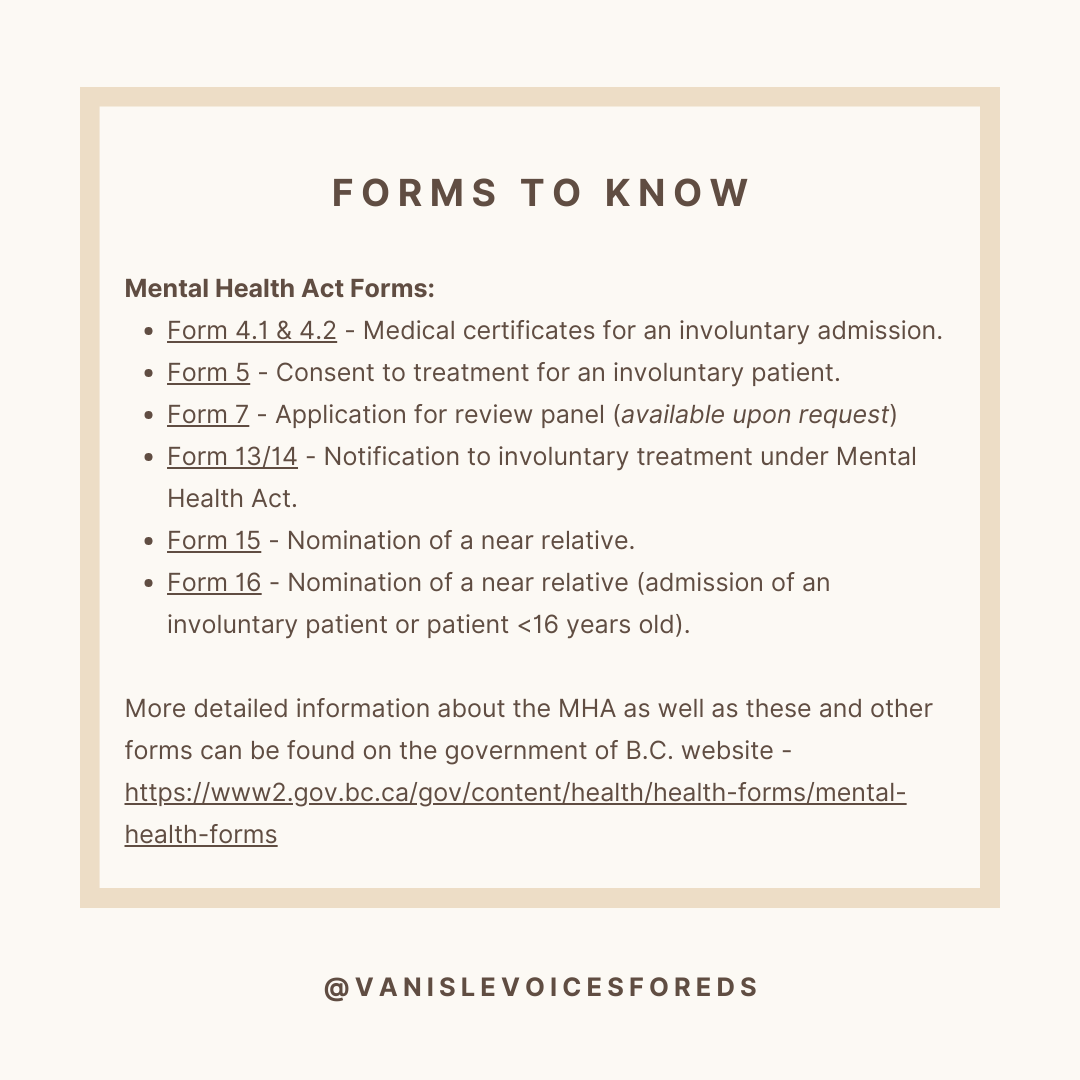
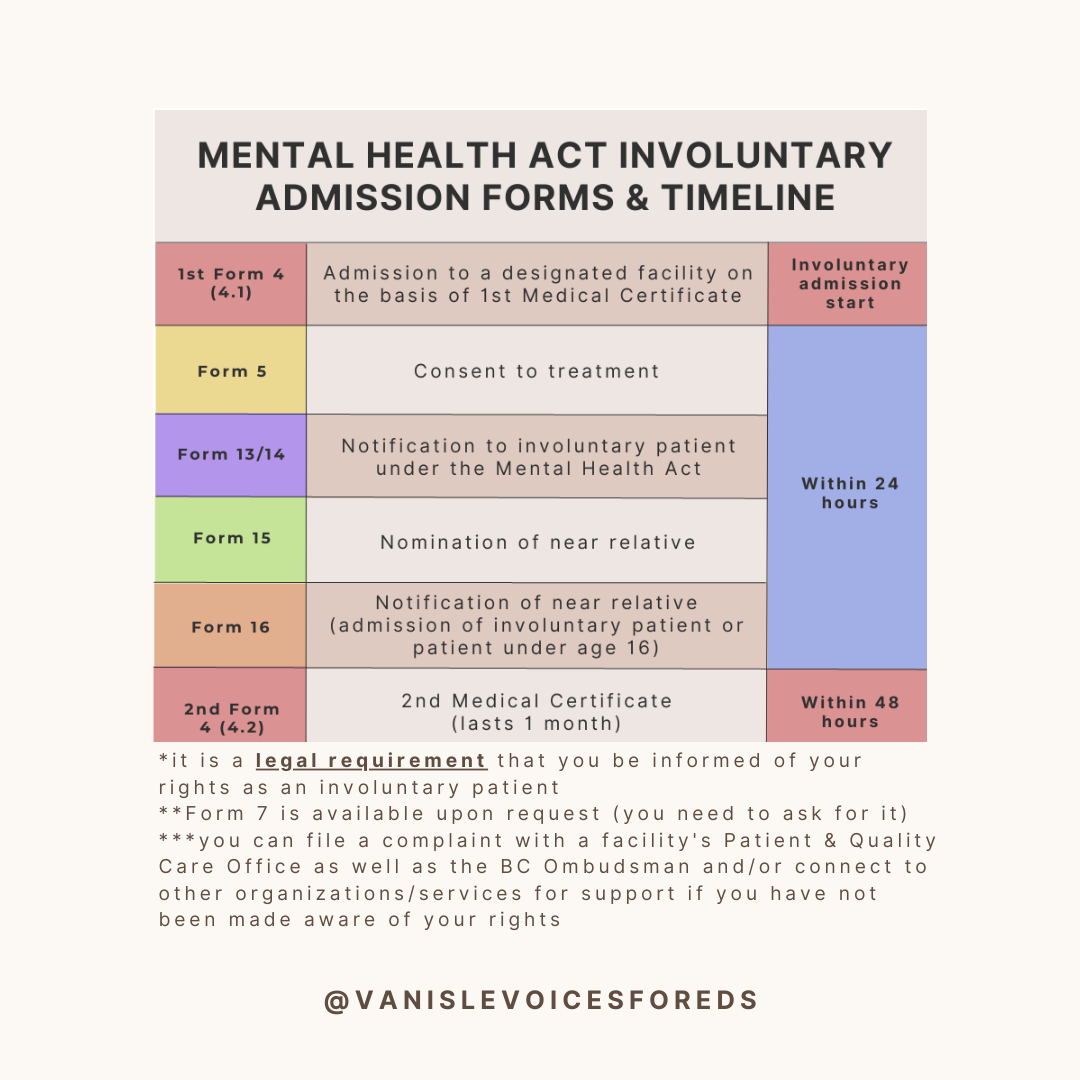
Mental Health Act Forms:
Form 4.1 & 4.2 - Medical certificates for an involuntary admission.
Form 5 - Consent to treatment for an involuntary patient.
Form 7 - Application for review panel (available upon request)
Form 13/14 - Notification to involuntary treatment under Mental Health Act.
Form 15 - Nomination of a near relative.
Form 16 - Nomination of a near relative (admission of an involuntary patient or patient <16 years old).
There is a free, downloadable wallet card that lists your rights under the Mental Health Act in BC
Health Justice & CMHA BC provide a joint service known as the Independent Rights Advice Service (IRAS) in many locations around the province. The service connects involuntary patients with a virtual rights advisor who is specifically trained to help explain what your rights are under the Mental Health Act (healthcare professionals do not have formal training on rights advice). If you are an involuntary inpatient request to access this service as it is independent from the hospital you are detained within. If you are on “extended leave” this service can also be contacted. See the following link for more information on how to connect with the IRAS.
Health Justice also has resources and information related to the Mental Health Act and your rights under the Act that can be useful to familiarize yourself with. Their organization uses research, education, and advocacy to improve the laws and policies that govern coercive mental health and substance use care in BC.
CMHA BC has helped to launch several Peer Assisted Crisis Teams (PACT) in BC with opportunities for expansion. In Victoria, AVI operates a local PACT (now called CLCR) that provides an alternative to police involvement and forced treatment.
Hours: 2 - 9 PM PST
Phone: 250-818-2454
(AVI also operates a mobile harm reduction service).
If you are in a healthcare role that is governed by the current Health Professions Act in B.C. (e.g. nurses, physicians, etc.), you are subject to being reported to your regulatory body under section 32.3 of the current HPA upon presentation to an acute care facility with a primary diagnosis of a mental illness or substance use.
If you have a union, they may be able to help support in navigating the return to work process and serve as an interface between you and your regulatory body.
You will need to provide a physician's approval to return to work and they may be required to complete follow up forms or questions.
A reminder for those in involuntary psychiatric care or who have gone through it - You are not a burden, you are not broken. You are a whole and complex human being; not a diagnosis or a problem that needs to be solved. You are a person who is worthy of dignified care who holds the capacity to heal even if it is hard to imagine in the moment. There are people and places who believe you and in you.
Form 20 - Extended Leave
"A Form 20 (Leave Authorization), also known as Extended Leave (EL), is a form under the British Columbia Mental Health Act that allows an involuntary patient to leave the hospital and live in the community.
Under this Form, a patient will return to live in the community, but are still legally considered an admitted and involuntary patient. Note that Extended Leave is not the same as a full discharge from hospital."
Certain conditions and requirements must be met in order for the extended leave to be maintained (otherwise an individual would be brought back to a designated facility).
Conditions might include things such as:
Taking a medication at a prescribed dose
Attending outpatient appointments
Keeping members of the team updated via routine check ins
Living in a certain, agreed upon location
Having travel or other plans pre-approved and planned around by the mental health team
An extended leave is often "intended" to be a way to promote patient autonomy where possible, while still ensuring recommended treatment is adhered to; however, intention is not the same as impact and there are significant implications that come with being place on an extended leave.
Inpatient psychiatric admissions can be highly traumatic and extended leave is no different in its potential risks - while people maintain basic rights under the MHA, to have a person living with such limited autonomy and bodily freedom should only ever be an absolute last resort - you are sentencing a person to live under the threat of constant forced treatment and detainment.
What you need to know about being under a form 20 (extended leave):
1. You have the right to know whether you are being discharged from a facility or being placed on extended leave and what that entails.
2. You have the right to know what conditions are a part of your extended leave.
3. You have the same rights on an extended leave as you do when you are an involuntary patient in the hospital or an equivalent healthcare facility.